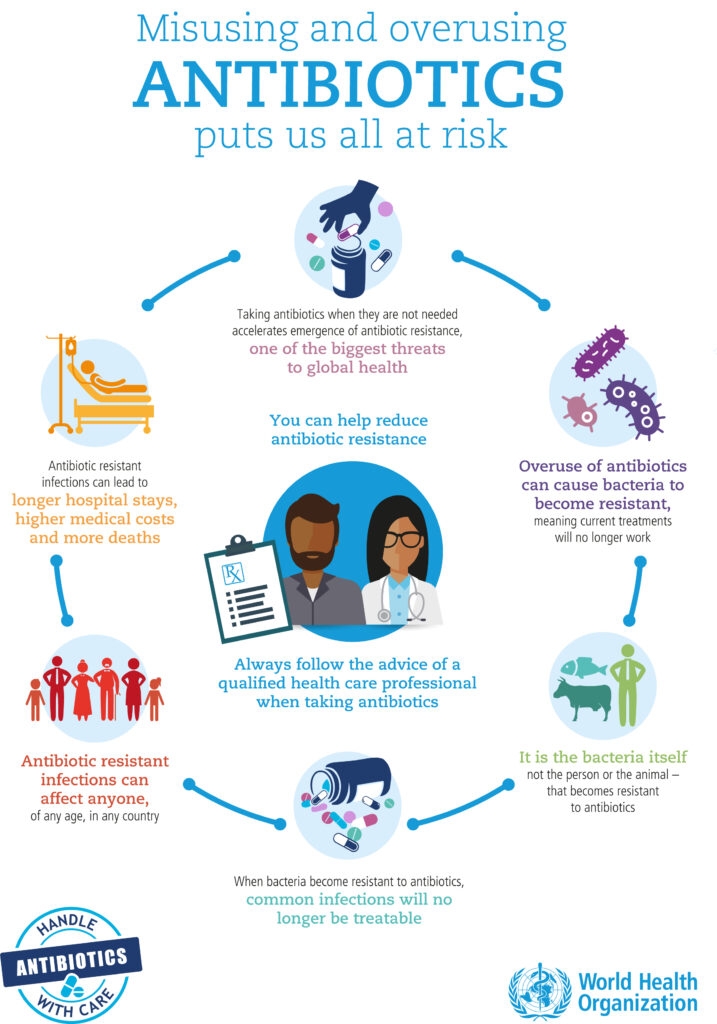
Antibiotics save lives, but antibiotic overuse is creating a serious health threat worldwide. Some medications that used to be standard treatment for bacterial infections are now less effective or don’t work at all. When bacteria in the body are exposed to antibiotics, they adapt to resist the effect of the drug. The more often that antibiotics are used, the faster this resistance develops. Antibiotic-resistant bacteria can then spread between humans and animals through direct contact, food, or the environment.
Read on to learn more…
BACTERIA vs VIRUS
There are two major types of bugs that make people sick: bacteria and viruses. While symptoms of infection may be similar, bacteria and viruses are actually very different:
Bacteria are tiny microorganisms that exist as a single cell. Bacteria are everywhere. Most bacteria are beneficial, and many are essential to life as we know it. Only a small handful of known bacteria are capable of causing disease. These bacteria are termed pathogenic. They cause illness by invading the body, multiplying, and interfering with normal bodily processes. Antibiotics work against bacteria because they kill these living organisms by stopping their growth and/or reproduction.
Viruses are another type of tiny microorganism. Unlike bacteria, viruses cannot live on their own. Instead, they are parasitic; viruses grow and reproduce only after they’ve invaded other living cells. The body’s immune system can fight off some viruses before they cause illness, but others – such as the common cold – must simply run their course. Antibiotics do not work against viruses.
Common viral infections that don’t benefit from antibiotic treatment include:
- Common cold
- Flu (influenza)
- Bronchitis
- Most coughs
- Some ear infections
- Some sinus infections
- Stomach “flu” viruses
OVERPRESCRIPTION
While some rapid diagnostic tools are available to help doctors discern between bacterial and viral infections, sometimes doctors aren’t sure if an illness is caused by bacteria or a virus. In these cases, they may prescribe an antibiotic when it isn’t necessary. Also some patients might expect a prescription for an antibiotic and will ask their doctor to write one. Pressure from patients can lead to doctors writing prescriptions for unnecessary antibiotics.
CONSEQUENCES
Taking an antibiotic for a viral infection won’t cure the infection, stop the spread of the infection to others, or improve how you feel. Antibiotics attack both helpful and harmful bacteria in your body. If you take an antibiotic when you have a viral infection, the antibiotic may create an opportunity for potentially harmful bacteria to replace the helpful ones. Taking an antibiotic for a viral infection may also cause unnecessary and harmful side effects and can change bacteria so that antibiotics are no longer effective.
Antibiotic resistance is a growing problem. The Centers for Disease Control and Prevention (CDC) calls it “one of the world’s most pressing public health problems.” It’s especially a concern in low-income and developing countries where access to antibiotics and vaccines is limited.
For many years, the introduction of new antibiotics outpaced the development of antibiotic resistance. In recent years, however, antibiotic resistance has created “superbugs”- a term coined to describe bacteria that cannot be killed using multiple antibiotics. Approximately 2 million infections from antibiotic-resistant bacteria occur in the United States each year, resulting in 23,000 deaths. Other consequences of medication-resistant infections can also lead to an increase in the length and severity of the illness, number of doctor visits, and cost of treatment.
PROPER USE
Every family faces its share of colds, sore throats, and viruses. When parents bring their children to the doctor for these illnesses, it’s important not to expect antibiotic prescriptions. To lower the risk of bacterial resistance and prevent antibiotic overuse, parents should let milder illnesses (especially those caused by viruses) run their course and refrain from pressuring doctors for antibiotic prescriptions.
Parents should also ensure antibiotics are used as prescribed, for the full duration of the prescription. It may be tempting to stop an antibiotic as soon as your child feels better, but full treatment is necessary to completely kill off the disease-causing bacteria. Failure to take an antibiotic as prescribed may lead to additional antibiotic treatment later and may promote the spread of antibiotic-resistant properties among harmful bacteria. Parents should never offer their child “leftover” antibiotics or ones that were prescribed for another family member or adult.
The appropriate use of antibiotics — often called antibiotic stewardship — can help to:
- Preserve the effectiveness of current antibiotics
- Extend the lifespan of current antibiotics
- Protect people from antibiotic-resistant infections
- Avoid side effects from using antibiotics inappropriately

HYGIENE/PREVENTION
Preventing sickness reduces the amount of antibiotics people use and the likelihood that antibiotic resistance will develop. Parents should keep their children up-to-date on their immunizations and home from school when they are sick. Parents should also teach and model proper hand washing.
Hand washing can prevent approximately one third of all diarrhea-related illnesses and about one fifth of all respiratory infections.
For more information on how you can fight antibiotic resistance, visit www.who.int/drugresistance